RENEW. RESTORE. RECLAIM.
-
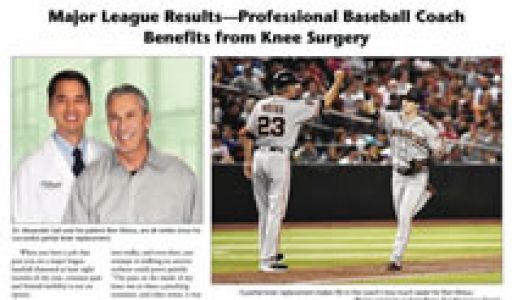
SF Giants 3rd Base Coach, Ron Wotus, shares his experience with partial knee replacement by Dr. Sah
-
Video Highlight- See Anterior Hip Replacement Patient Going Home Same Day of Surgery
-
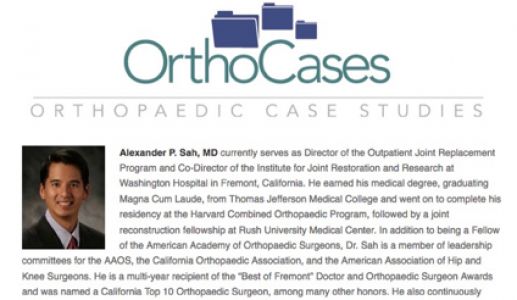
Dr. Alexander Sah is proud to be editor and author with Dr. Joel Matta on the definitive resource of national and international experts regarding advanced techniques in Anterior Hip Replacement, published in 2022.
-
As seen on ABC 7, Dr. Sah and Bay Area Healthier Together feature the program at the Institute for Joint Restoration
-
Dr. Alexander Sah is proud to serve as President of the Anterior Hip Foundation for 2022-23
-
Drs. Sah and Bonner are proud to offer the most advanced robotic-assisted knee surgery technologies to Bay Area. As the only surgeons with experience using robotic technologies at the Institute for Joint Restoration, this cutting-edge technology offers potential advantages over traditional techniques.
-
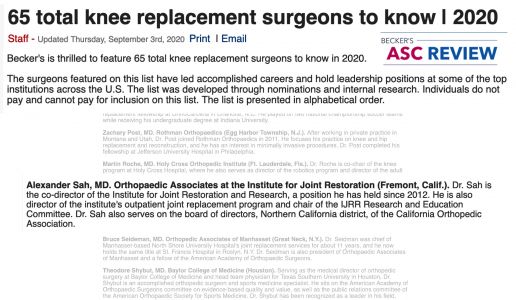
Dr. Sah selected to exclusive list as one of top knee surgeons in the nation by Becker's Review 2020
-
Dr. Sah and Dr. Bonner are the only surgeons currently, or ever, to perform Anterior Hip Replacement at the Institute for Joint Restoration
-
Dr. Sah presenting at the national AAOS Outpatient and Rapid Recovery in Joint Replacement course for Orthopedic surgeons in November 2022
-
Sah Orthopaedic Associates is delighted to welcome Bryant Bonner, MD as the newest associate to the team. Trained at the Harvard Orthopedic Residency program, he has expertise robotic knee surgery, anterior hip replacement, minimally invasive hip and knee replacement, and complex and revision hip and knee surgery.
-
Dr. Sah only surgeon performing Outpatient Total Hip and Total Knee replacement at Washington Outpatient Surgery Center
-
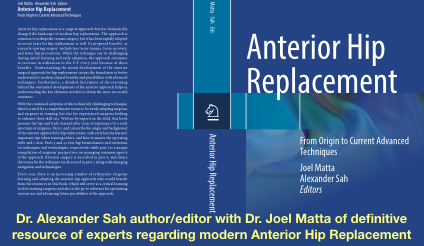
Anterior Hip Replacement- from Origins to Current Advanced Techniques, published 2022
-
Dr. Sah and Bay Area Healthier Together on ABC 7
-
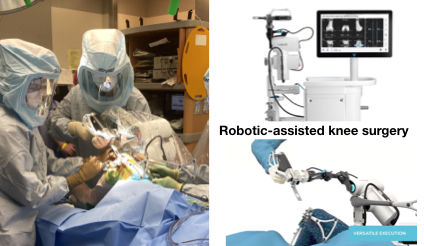
Robotic-assisted knee surgery
-

Video Highlight- See Anterior Hip Replacement Patient Going Home Same Day of Surgery
-
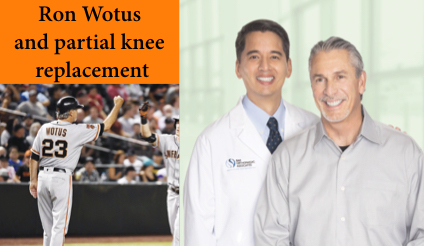
SF Giants 3rd Base Coach, Ron Wotus, shares his experience with partial knee replacement by Dr. Sah
-
Dr. Sah serves as President of the Anterior Hip Foundation 2022-23
-
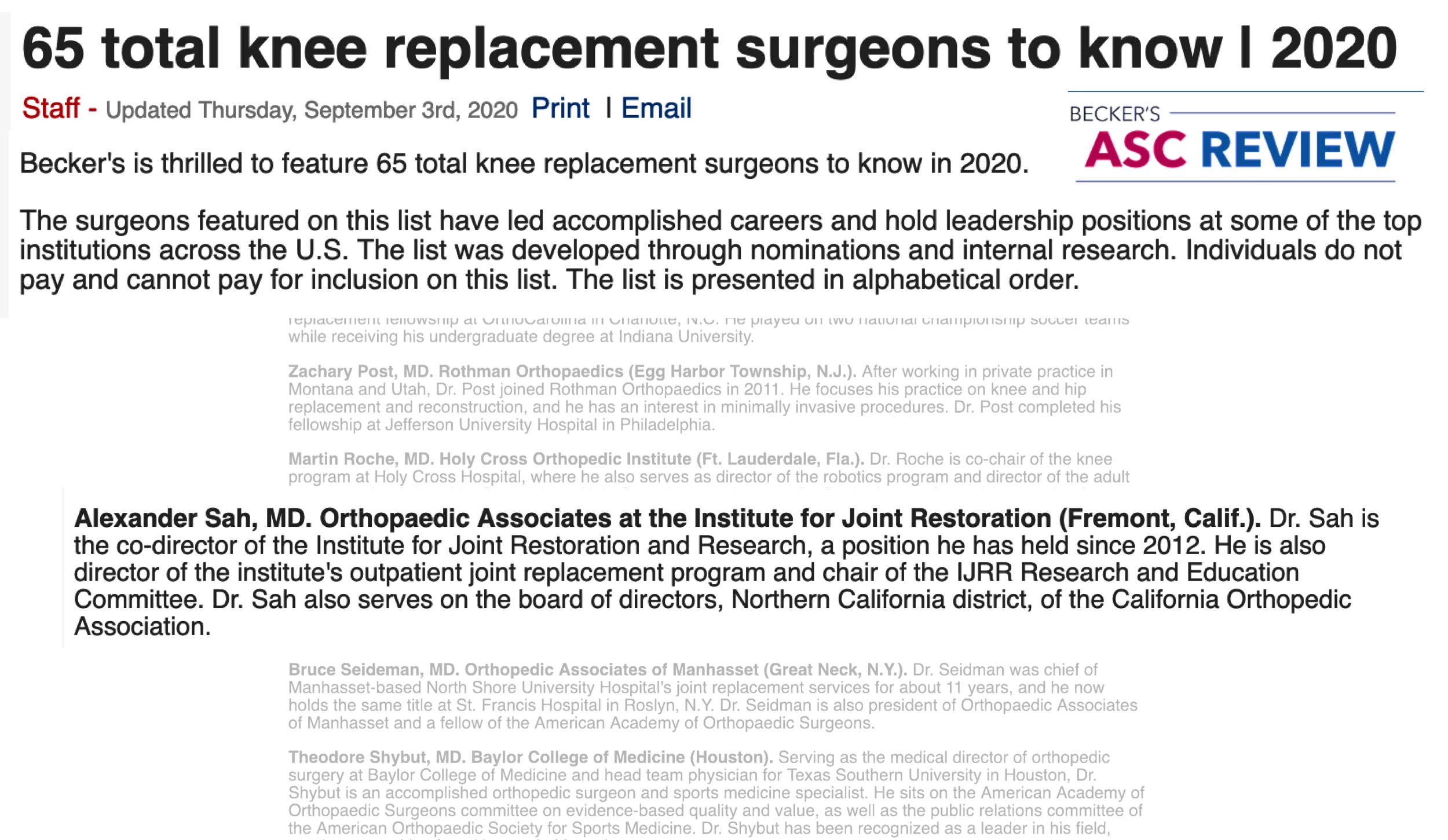
Becker's top surgeon list 2020
-

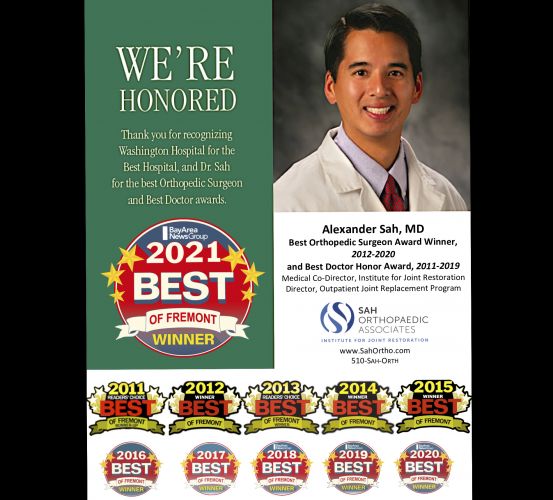
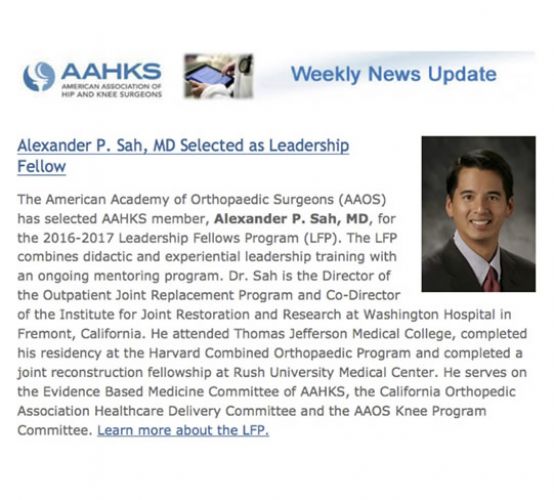
Best Doctor
-
JBJS
-

Americas Most Honored Professional
-
Orthopedic Review
-

Compassionate Doctor Award
- Anterior Hip Replacement- from Origins to Current Advanced Techniques, published 2022
- Dr. Sah and Bay Area Healthier Together on ABC 7
- Robotic-assisted knee surgery
- Video Highlight- See Anterior Hip Replacement Patient Going Home Same Day of Surgery
- SF Giants 3rd Base Coach, Ron Wotus, shares his experience with partial knee replacement by Dr. Sah
- Dr. Sah serves as President of the Anterior Hip Foundation 2022-23
- Becker's top surgeon list 2020
- Best Doctor
- JBJS
- Americas Most Honored Professional
- Orthopedic Review
- Compassionate Doctor Award
Welcome to Sah Orthopaedic Associates
Where state-of-the-art surgery meets unparalleled
personalized
care.
We are committed to delivering the highest quality joint replacement care possible, in the most compassionate way possible. Our team performs the most hip and knee replacement surgeries in Northern CA, and tops in CA and the West Coast. Yet, we also provide our patients the most personalized and individualized care available. Our comprehensive program is based on five pillars including: unique personalization, cutting-edge techniques and protocols, research & education, an integrated team approach, and an award-winning Institute for Joint Restoration facility. We hope that you find the information here helpful and informative.
What Our Patients Say
-
"Dr. Sah is my hero and has restored my faith in the fact that there are excellent doctors out there that are experts in their field and also care deeply about their patients. You just have to be lucky enough to find them, in this case, Dr. Sah! Dr. Sah recommended anterior hip replacement. I am thrilled to say he did a masterful job. The surgery was smooth and flawless. I was pain-free immediately and walking without a walker or cane in 2 days. I was very pleased and extremely impressed with Dr. Sah and his entire team. They are all so dedicated, caring and truly experts in their field. My entire experience was and continues to be exceptional. MY THANKS & GRATITUDE to Dr. Sah (& his team) for restoring my quality of life and for building an amazing practice that feels like a big happy family."
DM, San Jose
-
"Simply the BEST Hip and Knee surgeon! Dr Sah is a master at what he does.. and has made my experience pretty much free of fear and pain.. this is not your Mama's hip replacement for sure! Up and walking within a couple hours of surgery.. and slept in my own bed at home the same night!! Totally Amazing! Dr Sah and staff have this replacement gig down to a fine art! Thank you Dr Sah, your staff and the team at Washington Hospital for my wonderful new hip!"
SL, Moss Beach
-
"Thank you Dr. Sah and your tremendous staff. I am now 70, still pain free and very active again all because of SAH Orthopaedic Associates Institute for Joint Restoration. If you are contemplating this procedure, your search should end here for results that will restore your body and mind. I wish Dr. Sah was my neighbor so I could thank him everyday in person."
RH, Valley Springs
-
"I had a partial knee replacement from Dr Sah after 6 previous surgeries on my left knee. The results have been life changing. After more than 30 years of daily pain I'm pain free. The recovery was quick and I was riding a bike and playing golf within 3 months. Keys to the success were Dr Sah's skill, getting into the best shape I could beforehand, losing weight and not missing a day of physical therapy after. I highly recommend Dr Sah, not only as a surgeon, but also as a caring healer."
GF, Wastonville
-
"I met with 3 knee surgeons to discuss a partial knee replacement, 2 in Santa Cruz and Dr. Sah in Fremont. Dr. Sah was hands down the most professional and knowledgeable. Even thought I would have to drive an hour to see him and the surgery would not be in my local hospital, it was a no brainer to chose him. The surgery and everything leading up to it with Dr. Sah was an amazing experience. All surgeons could learn from how Dr. Sah treats and educates his patients. The after care was just as amazing. It has been almost 4 months since my surgery, I am able to surf again and the do other things in life that are important to me."
WS, Santa Cruz
-
"Dr Sah performed a complicated revision of my knee which involved replacing all the old hardware. My first replacement 10 years ago, with another Dr/facility, had always been a problem and eventually caused damage to the bone and soft tissue.. I could not be happier with the outcome of my current procedure. I also hold Dr Sah and his staff in the highest esteem. They give the highest quality care with compassion and visible caring. I got all the time I needed during visits for my questions and had my email questions answered within a day. I also received at least a couple of phone calls at home from Dr Sah to check in with me. He gives extra-ordinary care. I wish I had found Dr Sah much earlier."
ML, Los Gatos
-
"I cannot say enough about this outstanding surgeon. Dr. Sah makes you feel like a person and not just a patient as he spends the time to connect with you and understand your story. He even sent a hand written letter to me after my intro visit before he even knew I was choosing him to perform both hip replacements. He also would call me periodically after each surgery to see how I was progressing, showing me he really cared. I highly recommend Dr. Sah. He replaced my awful degrading hips and gave me my life back. I can walk swiftly now and started weight lifting again, especially my lower body. It doesn’t get sweeter than that. I can now walk around comfortably with a smile on my face like I was once able to do."
BC, Danville
-
"It's been a year since Dr. Alexander Sah replaced my right knee,and eight weeks after that,my left knee. I was,for all intents and purposes, facing a life in a wheelchair, unable to go back to my home, reduced, possibly, to passing my days in an assisted living facility. Dr. Sah changed that. He didn't give me back my life...he gave me back a better life. If I had not become Dr. Sah's patient,I have no doubt that today I would be struggling with a limited,pain-filled life,most likely no longer capable of living in the home that I love,but in a "manageable" living space,possibly no longer able to drive,certainly not to be fully independent. This knee surgery,and the splendid care I received during those long months,has truly been a life-changing gift."
ET, Berkeley
-
News
-
Anterior Hip Replacement- from Origins to Current Advanced Techniques, published 2022
Anterior Hip Replacement- from Origins to Current Advanced Techniques, published 2022 Dr.... -
Dr. Sah serves as President of the Anterior Hip Foundation 2022-23
Dr. Sah serves as President of the Anterior Hip Foundation 2022-23 The Anterior Hip Foundation... -
65 Total Knee Replacement Surgeons to Know | 2020
65 Total Knee Replacement Surgeons to Know | 2020 -
Dr. Sah and Bay Area Healthier Together on ABC 7
Dr. Sah and Bay Area Healthier Together on ABC 7 → Learn more about Dr. Sah and Bay Area...
-
-
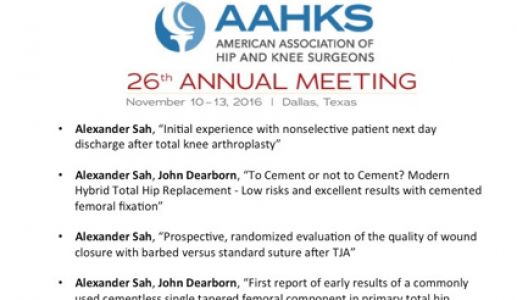
Research
-
Videos
-
In the press